Acne Treatment
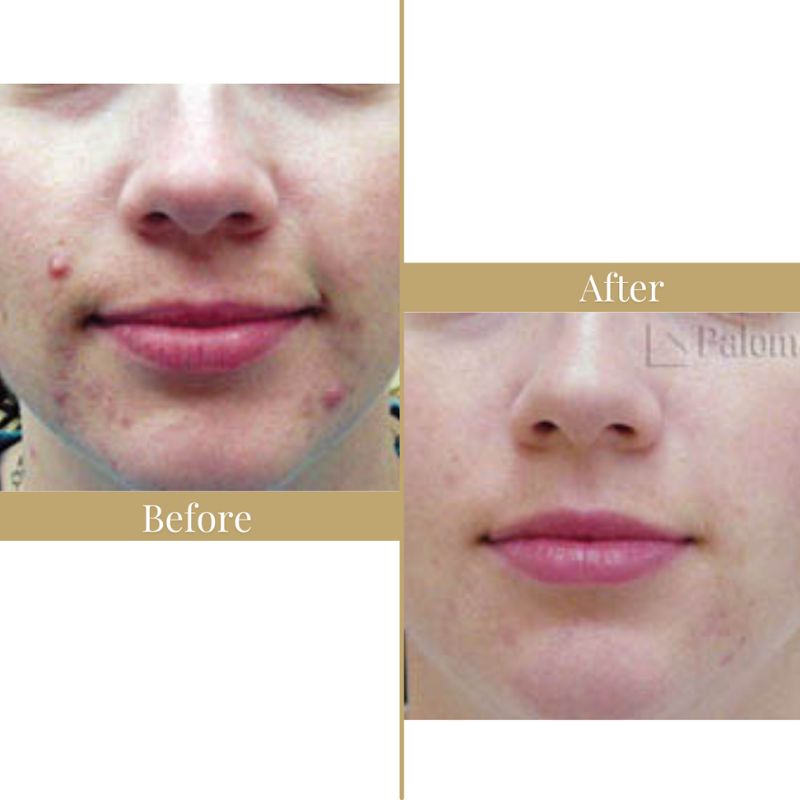
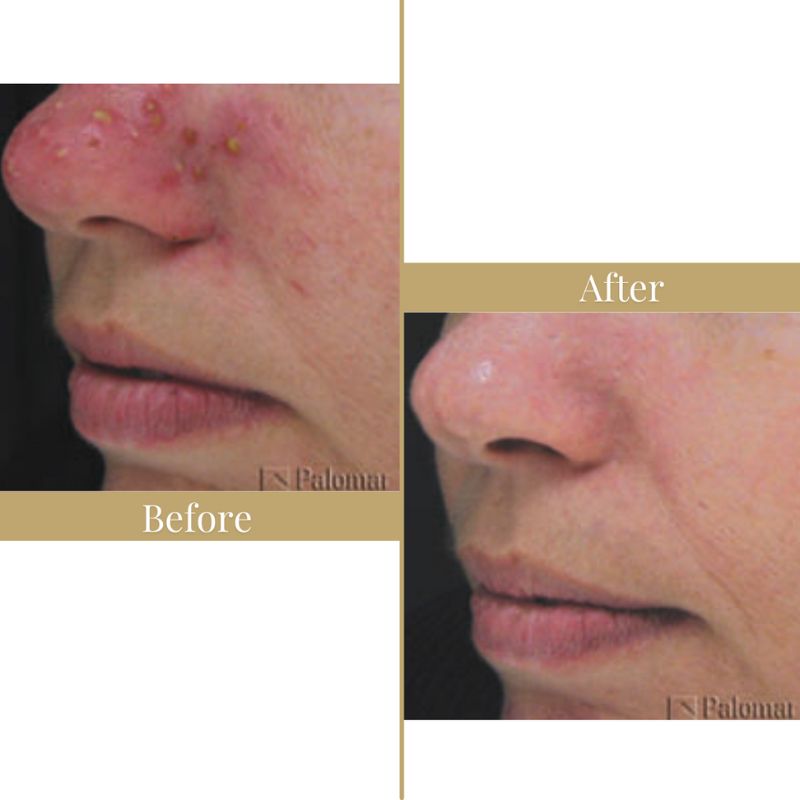
Acne is one of the misfortunes of adolescence. For some people skin blemishes occur in adult life as well. Acne is a skin condition that occurs when the oil-secreting glands in the skin are clogged and become inflamed or infected.
LustrePro Pure Light is the new Acne light treatment available at The DermaClinic Blackrock Dublin. LustrePro Pure light Acne treatment is developed by leading dermatologists and tested by healthcare professionals.
★★★★★
“I highly recommend The DermaClinic Blackrock, for over two years I have visited this Clinic. The Clinic Director Patricia Molloy is very knowledgeable and Highly professional”.
While not life threatening, acne can leave life-long emotional and physical scars — a reminder of the embarrassment and self-consciousness that came with the pimples. No one wants to get zits.
Approximately 90% of all adolescents and 25% of all adults experience acne at some point in their lives. It’s one of the most extensive medical conditions in the world, and is responsible for about 30% of all visits to the dermatologists. Unfortunately, it’s not easy to treat. Traditional therapies have a variety of side effects and sometimes require months to work, if they work at all. Oral antibiotics can cause stomach upset, light sensitivity and yeast infections in women, and studies indicate about 40% of skin bacteria have become resistant to antibiotics, making them a doubtful ally in the fight against skin breakouts.
Acne is a common, chronic skin condition caused by inflammation of oil-producing sebaceous glands. Acne usually begins between the ages of ten and thirteen, and persists for five to ten years. Acne breakouts are most common on the face, but they can also occur on the back, shoulders, neck, chest, scalp, upper arms and legs.
Young men and women get acne in equal numbers. Younger males are more prone to severe, longer-lasting forms of the skin condition. Many women suffer from “hormonal acne” — their outbreaks are tied to the hormonal changes related to their menstrual cycle. While hormonal acne typically starts between the ages of 20-25, it can strike teenagers as well. Hormonal acne is sometimes persistent in women in their 30s and 40s.
Even though teenagers tend to call any form of a breakout a “zit,” acne has more than one symptom. A build-up of P. acne’s can cause:
When left untreated, or when “picked at,” acne lesions can lead to permanent scarring.
How do we treat acne?
We offer a free consultation where detailed clinical assessment may be carried out to prescribe the appropriate treatment.
Single or combination treatment may be prescribes these may include:
There is a new paradigm for the treatment of acne. It involves a short treatment regimen with impressive results and no side effects, pain or downtime. ClearLight uses Acne PhotoClearing TM technology to destroy acne-causing bacteria within the skin. Applied in eight treatments over a four week period, most patients see a dramatic decrease in the number and severity of acne lesions; some report significant improvements after only two or three sessions.
See Acne Therapy Page for more information on Clearlight.

Light Therapy for Acne
LustrePro Light is the new Acne light treatment available at the DermaClinic Blackrock Dublin.
Acne affects 80% of people at some point in their life and can affect adults well into their 20s and 30, and some even older, and many seek drugs and antibiotics for their acne but these only tackle the symptoms and not the cause. Lustre Pure Light is a breakthrough technology that uses blue light technology to target acne bacterias directly at the source leaving your skin beautifully replenished and acne free
Scientists have found that visible blue light at a wavelength of 420 nm is effective in killing P. acnes, the bacteria which causes acne.
The DermaClinic has used Blue light for many years to treat acne. this home care kit Lustre Light is the latest in Acne treatment.
How does blue light kill the bacteria which cause acne?
The bacteria that cause acne produce a chemical called porphyrin. When blue light at a specific wavelength is applied to this porphyrin it becomes excited. This active porphyrin has been clinically proven to destroy the bacteria.
Lustre Pure Light treatment harnesses the safe, blue part of the natural light spectrum and the technology has been clinically proven to eliminate the bacteria that cause spots while also being gentle on the skin.
Lustre Pure Light emits light at 420nm and does not contain any of the ultraviolet light, which can damage skin.
How Lustre Pure Light works – the science
Step 1
Scientists have discovered that the spot causing bacteria, P. acnes produce a normally harmless chemical called Porphyrin.
Clinical trials have proven that when safe natural visible blue light at 420 nm is shone onto the skin there is no harm to the skin itself, but the Porphyrins produced by the spot causing bacteria become excited.
Step 2
When Porphyrins become excited they attach to the spot causing bacteria and begin to destroy it.
Step 3
When the spot causing bacteria P. acnes has been destroyed acne begins to clear and continued blue light use can help reduce P. acnes growth and stop new spots forming.
References used on this page:
Ref 1. Phototherapy with blue (415nm) and red (660 nm) light in the treatment of acne vulgaris. Papageorgiou et al British Journal of Dermatology 2000; 142:973-978.











